Dear Winston
It is inspiring to learn of your interest in sleep apnea. I will be happy to do my best to simplify, clarify and muddy your understanding of the AHI. AHI stands for Apnea Hypopnea Index. It is the standard for defining the presence of significant sleep disordered breathing and the condition of Obstructive Sleep Apnea.
It started long ago in the history of sleep medicine. In actual time, it was just 40-50 years ago. Physicians noted breathing problems during sleep. Over a decade or so it was clear from investigations that the problem was one of blockage of the airway in the throat during sleep. The blockage resulted in less air getting in and out of the lungs. The blood oxygen levels would drop, while the carbon dioxide level would increase. The sleeper responded with increased breathing efforts, which opened the airway. By the 1980’s, testing for these variables had evolved from investigative to the clinical practice level.
The AHI is the fundamental measurement for obstructive and central types of sleep disordered breathing. The A stands for apnea, or absence of breath. The H stands for hypopnea, or a critical reduction of airflow causing the same physiologic changes that the apnea produces. The I stands for index but actually represents a measurement of rate, the number of apneas and hypopneas per hour of sleep. The apnea as used in AHI represents the absences of air movement at the nose and mouth. Respiratory efforts by the diaphragm and chest may or may not be present. These are the simple definitions.
Clinicians and physiologists have much more specific definitions. Our definitions include the magnitude and duration of physiologic changes, as well as the types of equipment used for the measurements and the frequency of the changes. It should not surprise you that significant debate continues about the details of those changes. Opinions differ. Unfortunately, the efficient computerized testing systems we utilize, ease the burden of testing large numbers of people, but limit the ability to look at multiple variations of potential changes in definitions.
In this country, current technical definitions and the threshold for diagnosing the medical condition of apnea are cemented in place by the regulatory bodies; Medicare and commercial insurance companies set the standards. While the definitions set are supported by reported evidence, the standards are far from perfect and will not change soon.
The AHI is the gold standard for the definition of obstructive and central sleep apnea. Five events, apneas and or hypopneas, per hour of sleep meet diagnostic level for apnea. The level of 5 events was arrived at arbitrarily, based on early work in the field. Although accepted by those regulating groups, the actual minimal AHI needed to establish the diagnosis is not really known.
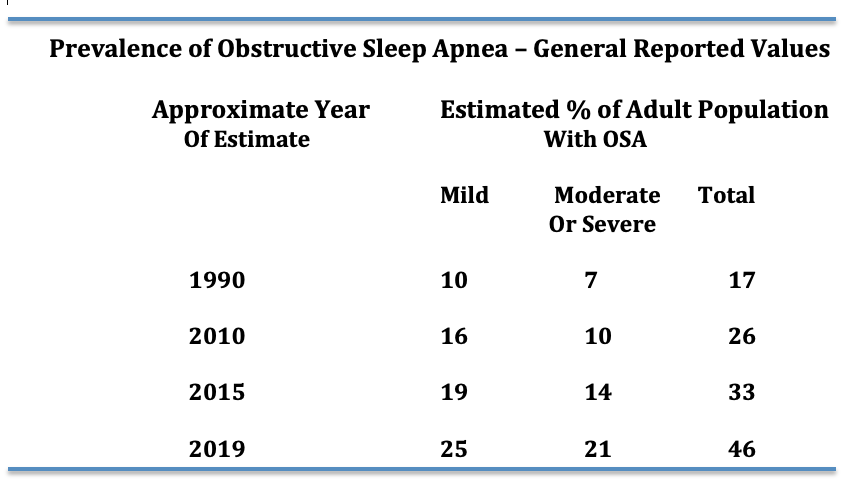
It is known that the higher the AHI the greater the risk for long-term medical problems. When a sleep study is complete and the AHI criteria for apnea is met, it is described as mild (5-15 events}, moderate (15-30 events) or severe (>30 events) apnea. The adjectives (mild, moderate and severe) represent the long-term risk for medical complications, not how a person feels. These separations into different severities of apnea, represent more tradition than science. In fact, the AHI is only a good predictor of severity for long-term complications at high levels (more complications) and very low levels (less complications). In the decades since these definitions for the onset and the severity of the disease were adopted, much research has been done. It appears that further definitions of these obstructive events would improve the accuracy of our diagnoses and the predictability of the future for the patient.
The current definitions have served time well. As a clinical tool, the AHI has proven to be extremely useful. It is accepted worldwide. Tremendous improvement in diagnosis and therapy for sleep apnea has occurred utilizing these measurements. There are limitations, however. This is specifically true when scientific studies of the condition are performed.
The role of low oxygen levels has been investigated more than any other factor. You will recall oxygen is measured on testing by the noninvasive transcutaneous method that reports oxygen saturations. Our technical definitions include a certain drop in oxygen saturation that is caused by the interruption to the airflow during the breathing events. The roles of the duration, severity and timing of the drop of oxygen in the sleep pattern as well as the total time spent at certain levels of oxygen desaturation are not known. Studies reviewing low oxygen levels during apnea suggest that the time spent with saturations of less than 90% together with the AHI is more accurate in predicting long-term medical complications than the AHI alone.
Another major factor not addressed with current testing is the use of a rate measurement for diagnostic purposes. A rate does not measure total exposure to apnea events. That is dependent on actual sleep time. An easy example is the difference of someone sleeping six hours versus another person who sleeps nine hours. They both can have the same AHI, but the person sleeping nine hours will be exposed to 50% more apnea events than the person who only sleeps six. The importance of exposure has not been studied at all.
The events we measure, apneas and hypopneas, do not occur uniformly throughout a night of sleep. The event frequency can change based upon body position. They can occur more while sleeping on the back verses the stomach. The events can occur more in REM sleep than in slow wave or Non-REM sleep. Research into the effects of these variables as predictors of long-term outcomes is limited.
Well, I believe it is time to close. The AHI is an immensely useful tool in the diagnosis and treatment of sleep apnea. It is the gold standard measurement for the diagnosis of sleep apnea. It needs to be improved upon and will be. As you will learn throughout your career, medicine changes slowly. Opinions are more rigid in medicine and in science than most believe. So, keep an open mind. This, like all things medical, will change with time.
RGH 7 April 2023 (28960)